Telestroke-Guided Intravenous Tissue-Type Plasminogen Activator Treatment Achieves a Similar Clinical Outcome as Thrombolysis at a Comprehensive Stroke Center
- We all know that intravenous thrombolysis has to become widespread to achieve any kind of success in our fight against stroke. However our efforts had been marred by the shortage of trained and certified neurologists who could thrombolyse. This new paper must be considered a landmark as it proves that IV thombolysis can be done
-
- Click to see the article abstract in the journal site
Telestroke-Guided Intravenous Tissue-Type Plasminogen Activator Treatment Achieves a Similar Clinical Outcome as Thrombolysis at a Comprehensive Stroke Center
- Syed F. Zaidi, MD;
- Mouhammad A. Jumma, MD;
- Xabier N. Urra, MD;
- Maxim Hammer, MD;
- Lori Massaro, CRNP;
- Vivek Reddy, MD;
- Tudor Jovin, MD;
- Ridwan Lin, MD, PhD;
- Lawrence R. Wechsler, MD
Correspondence to Lawrence R. Wechsler, MD, Professor and Chair, Department of Neurology, University of Pittsburgh, 3471 Fifth Avenue, 811 LK Building, Pittsburgh, PA 15213. E-mail wechslerlr@upmc.edu
Abstract
Background and Purpose—
Telestroke networks offer an opportunity to increase tissue-type plasminogen activator use in community hospitals.
Methods—
We compared 83 patients treated with intravenous tissue-type plasminogen activator by telestroke to 59 patients treated after in-person evaluation by the same neurologists at a tertiary care stroke center. Onset and door-to-treatment times and functional outcome at 90 days were obtained prospectively. Favorable outcome was defined as modified Rankin Scale score ≤2.
Results—
Favorable outcome rates were comparable between the groups (42.1% versus 37.5%, P=0.7). There was no significant difference in the rate of symptomatic hemorrhage.
Conclusions—
Telestroke is a viable alternative to in-person evaluation when stroke expertise is not readily available.
Results of MERCI trial paves the path for thrombolysis after 6 hours window...
- An interesting article
- All this time we have been following the dictum 'time is brain' although in practice a lot of patients have been benefited by thrombolysis after 6 hours. No the MERCI collaboratos have come out with with data to prove the same. A big thumbs up for them...It not only ahall pave the path for more patient oriented work, but also alter our thinking of the pathophysiology of stroke and the path our research should take.
-
- Original Contributions
Effect of Time to Reperfusion on Clinical Outcome of Anterior Circulation Strokes Treated With Thrombectomy
Pooled Analysis of the MERCI and Multi MERCI Trials
- Raul G. Nogueira, MD;
- Wade S. Smith, MD, PhD;
- Gene Sung, MD;
- Gary Duckwiler, MD;
- Gary Walker, PhD;
- Robin Roberts, BSc, MSc;
- Jeffrey L. Saver, MD;
- David S. Liebeskind, MD
- on Behalf of the MERCIMulti MERCI Writing Committee
+Author Affiliations
- From the Departments of Neurology, Neurosurgery, and Radiology (R.G.N.),
- Emory University School of Medicine, Marcus Stroke & Neuroscience Center,
- Grady Memorial Hospital, Atlanta, GA; Department of Neurology (W.S.S.), University of California,
- San Francisco, CA; Department of Neurology (G.S.), University of Southern California, Los Angeles,
- CA; Department of Interventional Neuroradiology (G.D.), University of California, Los Angeles,
- CA; Division of Clinical Research (G.W.), Concentric Medical Inc, Mountain View, CA;
- Department of Clinical Epidemiology & Biostatistics (R.R.), McMaster University, Hamilton,
- ON, Canada; Department of Neurology (J.L.S., D.S.L.), University of California, Los Angeles, CA.
- Correspondence to Raul G. Nogueira, MD, Emory Faculty Office Building 80 Jesse Hill Dr. SE, Room 398, Atlanta, GA 30303. E-mail rnoguei@emory.edu
Abstract
Background and Purpose—Previous studies have demonstrated a strong correlation between treatment time and outcomes after intravenous recombinant tissue-type plasminogen activator. However, the temporal profile of ischemia may vary according to the level of occlusion, and it is likely that more proximal occlusions have a more variable temporal course than their distal counterparts. We sought to establish how time influences outcomes in anterior circulation proximal arterial occlusions.
Methods—All patients from the MERCI/Multi MERCI trials with intracranial internal carotid artery and/or middle cerebral artery (M1-M2 segments) occlusions who were successfully revascularized were included in univariate/multivariate analyses to define the predictors of independent functional outcomes (modified Rankin Scale score ≤2) and mortality at 90 days. The effect of time to reperfusion on outcomes was calculated after adjustment for age, baseline National Institutes of Health Stroke Scale, and glucose levels.
Results—A total of 175 patients presenting with internal carotid artery/M1/M2 occlusions were revascularized. There was no definite association between time (to treatment or reperfusion) and outcomes in the unadjusted analysis. Baseline National Institutes of Health Stroke Scale score and age were independent predictors of independent outcome and mortality. High glucose demonstrated a strong trend toward worse outcomes. After adjustment for age, baseline National Institutes of Health Stroke Scale score, and glucose, there was a strong trend toward fewer independent outcomes with later reperfusion times. Notably, 40% of the patients reperfused at ≥6.9 hours achieved independent functional outcomes.
Conclusions—Time (to treatment or reperfusion) is only one of the many variables that may impact outcome in proximal arterial occlusions strokes. Reperfusion therapies should be started promptly, but our findings also suggest that stroke patients presenting at later time points may still benefit.
Key Words:
Curative embolization of brain arteriovenous malformations (AVM): Because We Could or Because We Should?
Brain AVMs for long had been enigmatic and 'touch me not' lesions, that is until some expert super confident vascular neurosurgeons started operating upon them, and some of them did pretty good job too. Also, radiosurgery ( gamma knife) has excellent results in a large number of these rather badly understood lesions. However, with the advent of smart endovascular neurointerventionists, they also started being treated by embolisation, initially as an adjunct to surgery of radiosurgery, and of late has been propagated as a single modality complete cure, especially with the advent and spread of ONYX.
However, the great interventional neuroradiologists advice a word of caution in following this approah.
Follow this link to see a good commentary by Jayaraman and Cloft.
http://www.ajnr.org/cgi/content/full/30/1/107
 jayaraman.png on Aviary.
jayaraman.png on Aviary.And here is an excellent reply to the above one from katsaridis
http://www.ajnr.org/cgi/content/full/30/5/e67
 katsaridis.png on Aviary.
katsaridis.png on Aviary.And here is an excellent comment in AJNR blog by the revered teacher Pearse Morris regarding the same point as Jayaraman.
This comment has incited a fantastic discussion on the above blog page among some of the biggest names in neurointervention.
http://www.ajnrblog.org/2009/02/02/embolization-of-brain-arteriovenous-malformations-for-cure/
 pearse morris.png on Aviary.
pearse morris.png on Aviary.And here is the link to the original article which started it all: the one by Panagiotopoulos et al
http://www.ajnr.org/cgi/content/short/ajnr.A1314v1
 panagiotopoulos.png on Aviary.
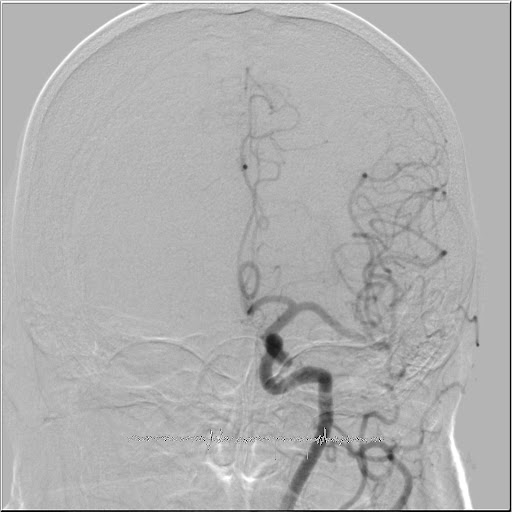
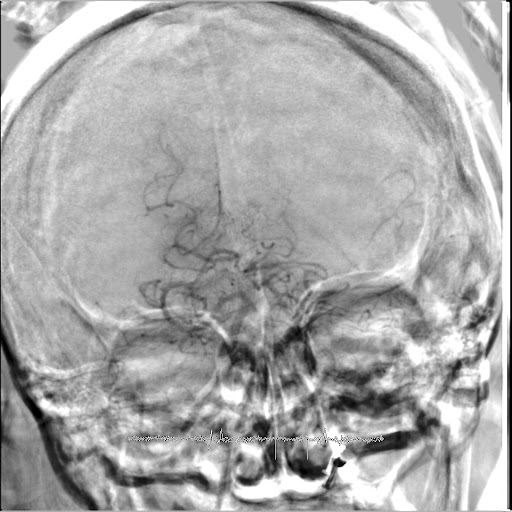
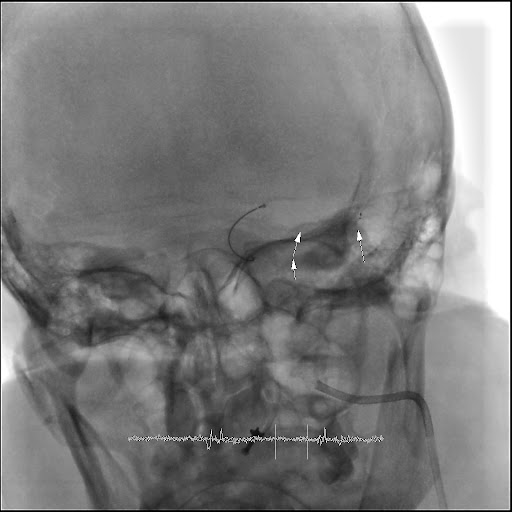
panagiotopoulos.png on Aviary.Mechanical Thrombectomy using SOLITAIRE FR stent system
For thrombectomy, the stent has to be inserted and used in the regular way. But after waiting for few minnuted for flow restoration to occur, the stent and the delivery microcatheter are pulled out from the guide catheter. The clot get entangled in the wall of the stent and comes out along with it. Multiple repeated passes of the stent may be needed before obtaining a satisfactoy result. Thus in practice it works like any other thrombectomy device.
Below is a case demonstration of the same.



Watch an animation of the Solitaire FR system
Below is a screenshot of the eV3 Solitaire FR information webpage










