Patient Resources: Foods that can trigger stroke...avoid them!
A good article on types of food which can trigger stroke. Stay away from them to avoid incidence of stroke...
Patient Resources: Coiling
What is coiling?
In the 1990s, coiling was introduced as a way of treating ruptured and unruptured aneurysms without the need for a craniotomy (an operation to open the head to expose the brain). Coiling involves approaching the aneurysm from inside the blood vessel, avoiding the need to open the skull. Small platinum coils are inserted into the aneurysm through the arteries that run from the groin to the brain. The coils remain in the aneurysm: they are not removed. They prevent blood flowing into the aneurysm and therefore reduce the risk of a bleed or a re-bleed. Blood then clots around the coils sealing off the weakened area. It is one of the most commonly performed and most rewarding procedures in interventional neuroradiology practice.What happens before the procedure?
The coiling procedure is similar to an angiogram (an X-ray test to take pictures of the blood vessels) and involves a very small tube (catheter) being fed up to the brain via blood vessels from the groin.However, it is much more complex and is usually carried out under general anaesthesia in the interventional neuroradiology department.
This means you must not eat or drink anything for four to six hours before the procedure. The staff on the ward will advise you on this.
Before you leave the ward, a nurse might shave a small area of your groin at the entry site through which the coils will be passed. If you are well enough, and if you prefer, you might be able to shave yourself.
On arrival at the radiology department, an anaesthetist will give you a general anaesthetic and you will be asleep throughout the procedure.
What happens during the procedure?
The room will have several large pieces of high-technology scanning equipment which are needed to perform the coiling.The interventional neuroradiologist will make a small incision in your groin through which they will insert the catheter into your femoral artery. This is then guided through other blood vessels in your body until it reaches your neck and then into your brain.
Using a guide wire and microcatheter, one by one, one or more coils are slowly inserted into the aneurysm. The coils are made of platinum, are twice the width of a human hair, and can vary in length. The number of coils needed depends on the size and shape of the aneurysm. The largest coil is inserted first and then smaller coils are inserted until the aneurysm is filled. Usually, several coils will be used.
After the whole aneurysm gets filled up by coils, the interventional neuroradiologist will remove the catheter. Occasionally, the entry point in the groin will need to be sealed or stitched. It might be slightly painful and there might be some bruising.
Coiling is a complex and delicate procedure that will take at least three hours and often longer.
What happens after the procedure?
You will probably spend some time in the high dependency unit – usually at least two hours. During this time, regular neurological observations will be performed by the nursing staff. This is to check that you are waking up properly from the anaesthetic. It involves asking you simple questions, testing the strength of your arms and legs, and shining a light in your eyes. Your blood pressure, heart rate, respiratory rate, and oxygen levels will also be monitored.The nurse will check the small wound in your groin for any bleeding and also check the pulse in your foot. This is to ensure that your blood circulation to your legs has not been affected.
It might be that the opening in your artery in your groin is plugged closed after the procedure. This is done with a device called an angioseal.
You will have to lie flat, or at an angle of no more than 30 degrees, for at least six hours following the procedure. This helps with your blood pressure and prevents any excess pressure on the artery which could increase the chance of bleeding at the puncture site in your groin.
Depending on your recovery after this time, you will be able to sit up gradually. The nurses will assist you with this.
Throughout this time, the nurses on the ward will continue to monitor you and carry out neurological observations. Pain-killers will be given for any discomfort or headaches you might be experiencing. You are also likely to have a drip to prevent dehydration, and possibly a urinary catheter.
Because you are restricted to bed rest, you will have to wear pressure stockings to help prevent blood clots forming in your legs (deep vein thrombosis).
What are the risks of coiling?
It is likely that the benefits of coiling will strongly outweigh any possible risks, and your doctor will have discussed this with you fully before you give your consent to go ahead with the procedure. However, as with any invasive procedure, there are certain risks associated with coiling. Possible complications include stroke-like symptoms such as weakness or numbness in an arm or leg, problems with speech, or problems with vision.There is also a risk of bleeding, infection or arterial damage at the entry site in the groin. In all the risk is not more than 3-4% and the risk of death is<1%.
How successful is coiling?
Research is still being conducted to explore the benefits and risks of coiling. Various studies have been published. The largest is the International Subarachnoid Haemorrhage Trial (ISAT) which was established to explore the effectiveness of coiling compared to the clipping of ruptured aneurysms during a craniotomy. The trial involved different neurosurgical centres and a total of 2,143 patients participated. The ISAT trial showed that the long-term risks of further bleeding are low for both coiling and clipping, and the results positively supported coiling as a treatment for ruptured aneurysms, both in terms of survival and in the reduction of long-term disability.Can the coils move?
Once the coils are securely in place they will not move out of the aneurysm.Will I need more coils?
Although the coils do not move, they might settle into the space within the aneurysm. This might mean that more coils are required to block off the aneurysm fully. This is why you will have a follow-up angiogram. Although in literature, about 15-20% patients have some refilling of the aneurysm, in our practice most of them do not need any further treatment. Around one in 20 patients require further treatment.Is it safe to coil aneurysms with difficult morphology?
The interventional neuroradiology practice has evolved rapidly along with the necessary expertise and the technological advances such that the things unthinkable of 10 years ago can be done now. e.g coiling of aneurysms with multiple sacs.
For aneurysms with large size or wide necks, balloon or stent support may be used. A wide variety of them are available now.
 Balloon assisted coiling
Balloon assisted coiling Stent assisted coiling
Stent assisted coiling Combined balloon and stent assisted coiling
Combined balloon and stent assisted coilingAn example of balloon assisted coiling is below.
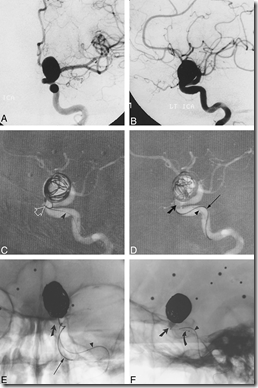

Fig: Balloon assisted coiling. A and B, Frontal (A) and lateral (B) arterial phase images from digital subtraction angiography (DSA) of the left internal carotid artery (ICA) show a large wide-necked aneurysm of the ophthalmic segment.
C and D, Road-mapped live subtraction images of the left ICA (lateral projection) show placement of the first coil. Note the herniation of a coil loop (arrow) through the neck of the aneurysm into the left ICA (C). In D, the balloon (thick arrow) has been inflated across the aneurysmal neck, permitting the framing coils to be deployed within the aneurysm. Arrowheads identify the indwelling 0.010-inch guidewire within the balloon microcatheter. An unextruded segment of a GDC (thin arrow) identifies the course of the coil-delivery microcatheter.
E and F, Frontal (E) and lateral (F) unsubtracted radiographs show deployment of a subsequent GDC. The images serve to orient the viewer with respect to the course of the ICA in relation to the aneurysmal base. The balloon (slanted arrow, E and F) has been inflated within the paraclinoid segment of the ICA, which sweeps lateral to medial across the face of the aneurysmal neck. The supraclinoid segment courses medial to the lower portion of the aneurysmal fundus and is partially obscured by the aneurysm in lateral projection. A small niche of aneurysm lying posterior to the ICA could not be angiographically thrown off the ICA by any of the views attempted. In this respect, the inflated balloon defines the boundary of the ICA lumen and assists the operator in coiling the aneurysmal base. The final segment of coil 14 (thin arrow, E) has been deployed in F. Note the alignment of the delivery wire marker with the proximal microcatheter marker (curved arrow, F). An indwelling 0.010-inch guidewire (arrowhead, E and F) identifies the course of the balloon microcatheter.
G, Mid-arterial phase image (frontal projection) from the immediate posttreatment left ICA DSA after deployment of the 18th GDC within the aneurysm. Coils are present throughout the aneurysmal base; however, minor opacification through the coil interstices is evident.
H and I, Frontal (H) and lateral (I) arterial phase images from the follow-up angiogram 18 months later confirm stable occlusion of the aneurysm.
New materials are being devised day to day e.g bioactive material coated coils which expand after deployment so as to prevent any chance of recurrence.
Patient Resources: Stroke
What is a
stroke/’brain attack’?
A stroke is the rapidly developing loss of brain function(s) due to disturbance in the blood supply to the brain.
A stroke is the rapidly developing loss of brain function(s) due to disturbance in the blood supply to the brain.
The traditional definition of stroke, devised by the World
Health Organization (WHO) in the 1970s, is a "neurological deficit of
cerebrovascular cause that persists beyond 24 hours or is interrupted by death
within 24 hours". This definition was supposed to reflect the
reversibility of tissue damage and was devised for the purpose, with the time
frame of 24 hours being chosen arbitrarily. The 24-hour limit divides stroke
from transient ischemic attack, which is a related syndrome of stroke symptoms
that resolve completely within 24 hours.With the availability of treatments
that, when given early, can reduce stroke severity, many workers now prefer
alternative terms, such as brain attack and acute ischemic
cerebrovascular syndrome, that reflect the urgency of stroke symptoms and
the need to act quickly.
What are the
types of stroke?
Stroke can be due to lack of blood flow (ischemia) =Ischemic Stroke, caused by blockage of an artery due to a clot within, or a hemorrhage (leakage of blood from the blood vessel) = Hemorrhagic stroke.
When a blood clot or a piece of atherosclerotic plaque (cholesterol and calcium deposits on the wall of the artery) lodges in an artery of the brain, it blocks the flow of oxygen-rich blood. The clot can develop in the brain artery itself (Thrombotic stroke) or can travel with the blood flow from another site like heart or another large blood vessel (Embolic stroke).
A cerebral hemorrhage occurs when a blood vessel in the brain bursts and bleeds into the surrounding brain tissue.
Stroke can be due to lack of blood flow (ischemia) =Ischemic Stroke, caused by blockage of an artery due to a clot within, or a hemorrhage (leakage of blood from the blood vessel) = Hemorrhagic stroke.
When a blood clot or a piece of atherosclerotic plaque (cholesterol and calcium deposits on the wall of the artery) lodges in an artery of the brain, it blocks the flow of oxygen-rich blood. The clot can develop in the brain artery itself (Thrombotic stroke) or can travel with the blood flow from another site like heart or another large blood vessel (Embolic stroke).
A cerebral hemorrhage occurs when a blood vessel in the brain bursts and bleeds into the surrounding brain tissue.
What are the features of stroke?
A stroke is a medical emergency and can cause permanent neurological damage, complications, and death. Stroke symptoms typically start suddenly within minutes and in most cases do not progress further. The symptoms depend on the area of the brain affected. The most common symptom is weakness (paralysis) of one side of the body. There may be partial or complete loss of voluntary movement of and/or sensation in a leg and/or arm. A stroke can result in speech problems and weakens muscles of the face, which can cause drooling. Numbness or tingling is very common. A stroke can cause difficulty inbreathing and even unconsciousness. The more extensive the area of brain affected, the more functions that are likely to be lost.
A stroke is a medical emergency and can cause permanent neurological damage, complications, and death. Stroke symptoms typically start suddenly within minutes and in most cases do not progress further. The symptoms depend on the area of the brain affected. The most common symptom is weakness (paralysis) of one side of the body. There may be partial or complete loss of voluntary movement of and/or sensation in a leg and/or arm. A stroke can result in speech problems and weakens muscles of the face, which can cause drooling. Numbness or tingling is very common. A stroke can cause difficulty inbreathing and even unconsciousness. The more extensive the area of brain affected, the more functions that are likely to be lost.
Silent stroke: A silent stroke is a stroke that does not have any outward symptoms, and the patients are typically unaware they have suffered a stroke. Despite not causing identifiable symptoms, a silent stroke still causes damage to the brain, and places the patient at increased risk for both transient ischemic attack and major stroke in the future. Conversely, those who have suffered a major stroke are at risk of having silent strokes. Silent strokes are estimated to occur at five times the rate of symptomatic strokes.
Some forms of stroke can cause additional symptoms. For
example, in intracranial hemorrhage, the affected area may compress other
structures. Most forms of stroke are not associated with headache, apart from
subarachnoid hemorrhage and cerebral venous thrombosis and occasionally
intracerebral hemorrhage.
How is a stroke diagnosed?
Anyone suspected of having a stroke should be taken to a medical facility immediately for evaluation and treatment. Other causes that can mimic a stroke include brain tumors, subdural hematomas (collections of blood between the brain and the skull), or brains abscess (a collection of pus in the brain caused by bacteria or a fungus). Viral encephalitis can cause symptoms similar to those of a stroke as can an overdose of certain medications. Following tests are generally carried out in the assessment of a stroke.
Anyone suspected of having a stroke should be taken to a medical facility immediately for evaluation and treatment. Other causes that can mimic a stroke include brain tumors, subdural hematomas (collections of blood between the brain and the skull), or brains abscess (a collection of pus in the brain caused by bacteria or a fungus). Viral encephalitis can cause symptoms similar to those of a stroke as can an overdose of certain medications. Following tests are generally carried out in the assessment of a stroke.
Routine testing stroke patients:
- Full blood count
- Blood glucose
- Blood urea, electrolytes
- Chest radiograph
- ECG
- CT scan
- Blood coagulation profile
Urgent CT scan of
the head is mandatory in all acute stroke patients. It is easily available,
very fast and serves the purpose in most patients. In some cases the physician
may ask the patient to undergo and MRI scans as well.
Risk factors
for stroke:
- Arterial Hypertension ( high BP)
- Cigarette smoking
- Diabetes mellitus
- Hyperlipedaemia
- Polycythaemia
- Thrombocythaemia
- High alcohol intake
- Positive family history
- Oral contraceptives
- Trauma
Stroke without an obvious explanation is termed
"cryptogenic" (of unknown origin); this constitutes 30-40% of all
ischemic strokes.
- Antinuclear factor
- Anti-bodies to double-stranded DNA
- Anti-cardiolipin antibodies
- Lupus anti-coagulant
- Cholesterol
What is the
treatment for stroke?
Early assessment of stroke is essential in order to start the appropriate therapy and limit, if possible any further damage due to stroke.
Early assessment of stroke is essential in order to start the appropriate therapy and limit, if possible any further damage due to stroke.
- Careful nursing
Regular turning of a patient to avoid pressure sores; skin kept dry and clean - Care of airway
Oropharyngeal tube with regular suction of secretions if the patient is unconscious - Fluid balance
Nasogastric feeding if patient cannot swallow; bladder catheterisation if incontinent - Physiotherapy
Start immediately to prevent joint contractions; to clear chest secretions; to promote recovery of strength and coordination - Speech and occupational
therapy
Start once acute stage over to assess functional problems and to encourage recovery skills
The blood sugar (glucose) in diabetics is often quite high
after a stroke. Controlling the glucose level may minimize the size of a
stroke. Before long, drugs that can actually dissolve blood clots may have a
place in stroke treatment. Oxygen is administered when necessary. New
medications that can help oxygen-starved brain cells survive, while circulation
is re-established, are being developed.
When a patient is no the mend after a stroke, the health care staff turns toward maximizing the patient's functional abilities. The rehabilitation process can involve speech therapy to relearn talking and swallowing, occupational therapy for regaining dexterity of the arms and hands, physical therapy for improving strength and walking, and family education to orient them towards caring for their loved one at home. The goal is for the patient to resume as many if not all of their pre-stroke activities and functions.
When a patient is no the mend after a stroke, the health care staff turns toward maximizing the patient's functional abilities. The rehabilitation process can involve speech therapy to relearn talking and swallowing, occupational therapy for regaining dexterity of the arms and hands, physical therapy for improving strength and walking, and family education to orient them towards caring for their loved one at home. The goal is for the patient to resume as many if not all of their pre-stroke activities and functions.
Active treatment of stroke:
Depending upon the type of stroke and the clinical
evaluation findings, the physician decides the further active treatment plan.
- Ischemic stroke: Clot busting medications can be given intravenously to dissolve the clot in the arteries so that blood flow is restored. Prior to it the physician evaluates the patient for suitability for ‘thrombolysis’. In certain patients, intraarterial therapy (done by interventional neuroradiologists) can be done to dissolve or retrieve the clot out of the blood vessel. Some patients may not be found suitable for either therapy however and they will be put on blood thinning drugs( antiplatelets or anticoagulants)
- Hemorrhagic stroke: Depending upon the type of hemorrhage the physician will decide the further active treatment e.g for subarachnoid hemorrhage; a DSA is done which usually shows an aneurysm and can be treated by interventional neuroradiologists by endovascular coiling. If there is a large intraparenchymal hemorrhage then open surgery to remove the clot and relieve pressure on the normal areas of the brain can be undertaken (craniotomy) by a neurosurgeon.
A: DSA showing an aneurysm of an
artery called anterior communicating artery, a very common site of involvement
B: Endovascular coiling has been
done. DSA after coiling shows complete packing of the aneurysm thus preventing
chances of re-bleeding
How can stroke be prevented?
One way to prevent a stroke is to notice a transient
ischemic attack (TIA) - or mini stroke - that provides symptoms similar to
stroke. Knowing the symptoms of stroke can lead to earlier treatment and better
recovery.
Much of stroke prevention is based on living a healthy lifestyle. This includes:
Much of stroke prevention is based on living a healthy lifestyle. This includes:
- Knowing and controlling blood pressure
- Finding out if you have atrial fibrillation
- Not smoking
- Lowering cholesterol, sodium, and fat intake
- Following a healthy diet
- Drinking alcohol only in moderation
- Treating diabetes properly
- Exercising regularly. Moderate aerobic fitness can reduce stroke risk,
- Managing stress
- Not using drugs
- Taking preventive medications such as anti-platelet and anticoagulant drugs to prevent blood clots
- Cholesterol lowering drugs can prevent stroke recurrence
- Secondary prevention of stroke: means ‘to prevent re happening of stroke after the patient has recovered from the present episode’. The patient will undergo some form of angiography (CTA, MRA or DSA) to have a look at the blood vessels If any narrowing is found then ‘angioplasty’ and ‘stenting’ may be offered by the interventional neuroradiologist.