proptosis on opposite side of carotico-cavernous fistula
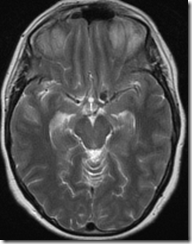
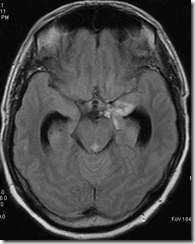
A 65 years old male patient had vision problems following head injury. Examination suggested a cortical type involvement and was confirmed on MRI as right PCA territory infarct
Fig 1: CT head and MRI T2WI showing chronic right PCA territory infarct
Fig 2: Axial and Coronal CT orbit does not show any definite e/o fracture
The patient was managed on conservative lines.
After a year he had sudden development of left orbital swelling and proptosis
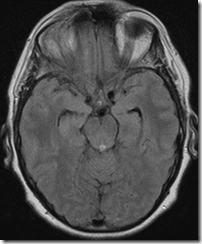
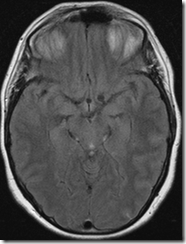
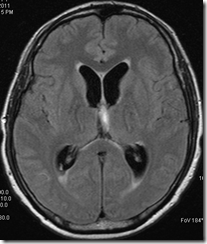
Fig 3: Axial T2W MRI images showing left proptosis; note the prominent superior ophthalmic veins which prompted for a DSA
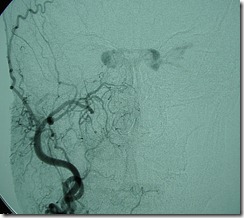
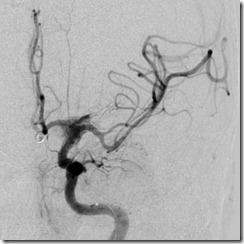
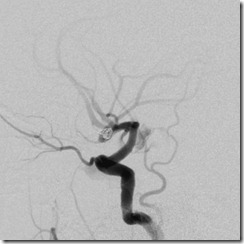
Fig 4: DSA showing direct type of RIGHT CCF. Prominent intercavernous venous channels connect to the ipsilateral cavernous sinus to the opposite side from which the LEFT ophthalmic veins fill retrogradely and produce the proptosis. Ipsilateral cavenous sinus also fills but to smaller extent. Also note the reflux into the deep venous system which makes this fistula a dangerous one.
Such findings are not uncommon although most patients will also have clinical manifestations on same side also.
What is rare is the fact that this patient came after a year with proptosis, probably a small aneurysm had developed and ruptured later on.
Spontaneous bilateral internal carotid artery occlusion
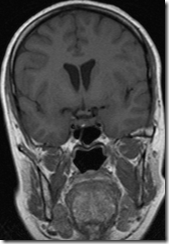
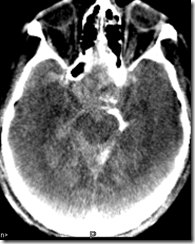
Case: A 48 years old female patient, previously healthy, presented with right hemiparesis which improved rapidly over two days with some residual weakness. She was found to have left perforator infarct on CT, and a doppler study showed absence of bilateral ICA flow.
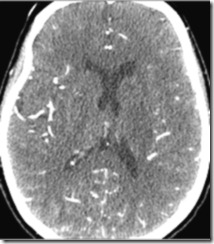
Fig1: CECT (actually source image of CTA) showing left gangliocapsular infarct
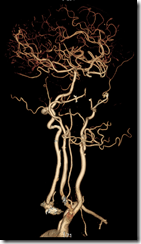
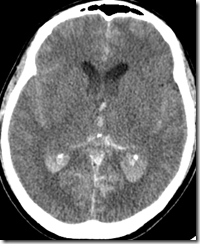
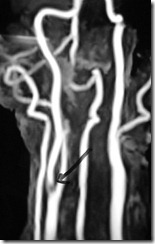
CT Angiogram was done which confirmed bilateral ICA occlusion.
Fig 2: CTA; 3D color SSD images; AP and oblique views; both internal carotids are completely occluded – right one from origin while on the left side a small stump is seen, right vertebral artery is dominat, left vertebral artery is hypoplastic, entire brain in almost dependent upon a solitary vessel –right vertebral, patent circle of Willis saving the patient from any major catastrophe with supratentorial parenchyma being supplied via posterior and anterior communicating arteries.
Discussion:
Spontaneous ICA dissection is an uncommon but increasingly recognized entity, with the increased awareness among physicians and the advent of modern imaging technologies, especially USG (and doppler) which is fast, ubiquitous and cheap.
Cervicocephalic dissections may occur spontaneously or secondary trauma which may be major but many patients have only minor trauma, something like playing cricket, yogasana, hiccups etc, while many housewives don't exactly recollect even trivial injuries. In some patients, they are associated with an underlying arteriopathy like
- Fibromuscular dysplasia, vessel tortuosity , Marfan syndrome , Ehlers-Danlos syndrome, Alpha-1-antitrypsin deficiency, Cystic medial necrosis, Type 1 collagen point mutation, Other connective tissue disorders
- In many, no cause of spontaneous dissection is found.
- systemic infections, hypertension, elevated homocysteine, alcohol, OCP have also been associated..
The cervical internal carotid artery is affected in 75% of patients (usually approximately 2 cm distal to the bifurcation) and the extracranial vertebral artery in 15%. The remaining cases usually involve the intracranial internal carotid artery, intracranial vertebral artery, middle cerebral artery, or basilar artery. Anterior cerebral arteries have been traditionally considered resistant, however modern imaging esp. DSA has found dissections in them too.
15% of cases are bilateral, and one half of these occur in patients with underlying fibromuscular dysplasia.
Age/Sex: Females> males, young- middle aged; cervicocephalic dissections are responsible for 1-2.5% of ischemic strokes in the general population and for 5-20% of strokes in individuals younger than 45 years.
Clinical features: commonest-focal unilateral headache; common- focal cerebral ischemic symptoms, oculosympathetic paresis, bruits, light-headedness, and neck pain; less common- syncope, amaurosis fugax, scalp tenderness, swelling in the neck, and dysgeusia
*Cephalic pain is frequent and often inaugural in carotid dissection; its recognition is important for early diagnosis and treatment, many also have painful Horner’s syndorme.
Cerebral ischemia occurs in at least 75% of reported cases (TIAs in 30%, infarcts in 45-50%).
Imaging: fat sat axial T1WI on MR very well show the dissected artery with hematoma and thrombus
Puppy sign in bilateral ICA dissection
J Neurol Neurosurg Psychiatry2007;78:1055 doi:10.1136/jnnp.2007.115857
However, sometimes MRI, MRA and Doppler will miss the dissections, and DSA is still the best for diagnosing as well as planning treatment.
Further reading:
- Mokri Bahram et al. Spontaneous dissection of the cervical internal carotid artery. Annals of Neurology. http://dx.doi.org/10.1002/ana.410190204

- Lucas C, Moulin T, Deplanque D, Tatu L, Chavot D. Stroke patterns of internal carotid artery dissection in 40 patients. Stroke 1998;29: 2646-8. [PubMed]
- Bradley Scott Townend, Laura Traves, Denis Crimmins, Bilateral spontaneous carotid artery dissection, Journal of Clinical Neuroscience, Volume 12, Issue 5, June 2005, Pages 592-594, ISSN 0967-5868, DOI: 10.1016/j.jocn.2004.08.020. (http://www.sciencedirect.com/science/article/B6WHP-4G1PKN8-8/2/c30c4ff302aaca48e64cc69e26ee967e)
READ THE IMAGING CORRECTLY 2: MISSED ANEURYSM
A middle aged patient had history of neck and occipital pain and presented to the neurologist who ordered an MRI cervical spine and brain. The report came as degenerative spine (Fig 1) and normal brain (Fig 2). the neurologist ordered physiotherapy and medications.
Patient had again transient LOC a month later.
An MRI brain was ordered which again was reported normal and patient was exhaustively investigated for various conditions, all of which were within normal limits.
A month and half later patient came to casualty with unconscious for 4 hours. An NCCT head was done which was reported as SAH.
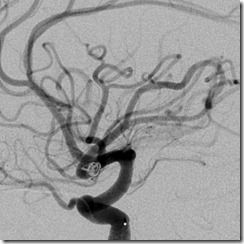
A DSA was done which showed left ophthalmic ICA aneurysm which was promptly coiled.
Patient was declared dead two days later.
Now lets review the images again:
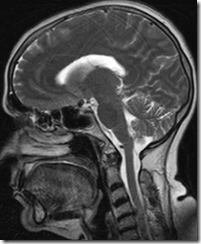
Fig 1: MR cervical spine, sagittal section, T1WI, showing the degenerative changes
Fig 2: Axial FLAIR image done on first visit, reported normal, shows the aneurysm very well
Fig3: MR brain done on 2nd visit very well shows the aneurysm on all planes and in all sequences
Fig 4: NCCT head, at admission on 3rd visit, shows subtle supratentorial brain parenchymal swelling and the ‘reversal sign’ suggestive of diffuse hypoxia with a ‘brain dead’ state probably already setting in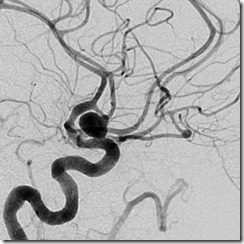
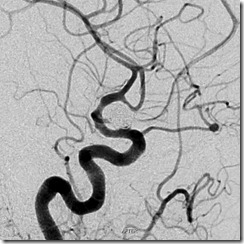
Fig 5: DSA images, pre and post –coiling, showing ophthalmic ICA aneurysm.
The images tell the entire story and also the sorry state of present medicine: both the radiologist and the neurologist had missed the lesion(s) repeatedly
ruptured SCALP AVM with large recurrent hematoma in A CHILD
A 3 years old child’s parents noticed a small swelling on the head at 2 months of age. the swelling increased gradually in size for a year then spontaneously decreased over a year. Following trivial fall, the swelling increased dramatically 3 days prior to presentation. He was otherwise normal.
On examination, the swelling was firm, smooth and pulsatile. No change related to posture or crying was seen.
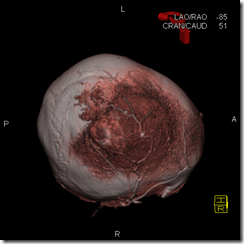
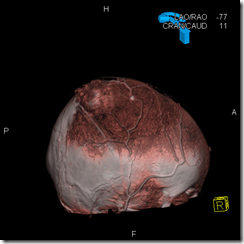
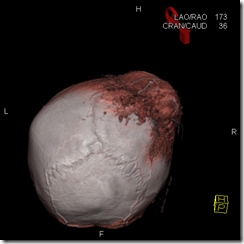
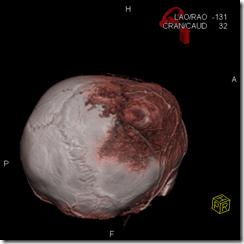
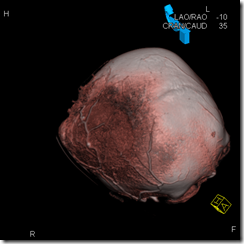
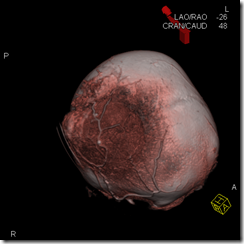
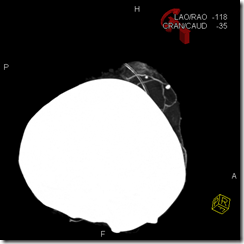
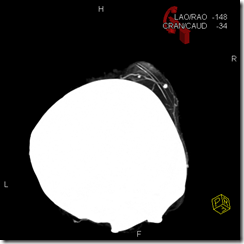
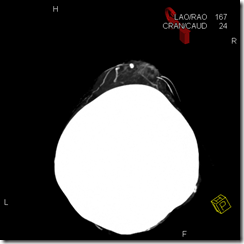
A CTA was done.
CTA, SSD and MIP images showing the right parietal swelling (hematoma) with a small AVM posteriorly, fed by branches of right superficial temporal artery. the feeders are elevated by the swelling. Also seen are a couple of phleboliths.
The AVM per-se was not filling a lot with contrast, probably partially thrombosed.
The baby was given antiinflammatory drugs and called for AVM excision after the hematoma resolved subsequently.
internal carotid artery perforation by microguidewire during acomm aneurysm coiling
43 years old male patient had a ruptured Acomm artery aneurysm and came for coiling after 1.5 months.
the first coil was successfully placed, however there was stretching of the second coil hence it was removed along with the microcatheter.
Subsequently a fresh catheter was intriduced over a microwire. During the manipulation, contrast leakage was noted from the supraclinoid ICA
LICA injection AP and Lat views showing contrast extravasation from terminal ICA. Note that the micocatheter has been pulled down now
Fortunately, the extravasation stopped spontaneously and rather quickly.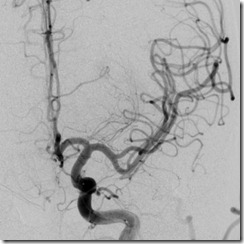
LICA injection after 3 minute of perforation, AP and Lat views, showing normal arteries with no e/o leakage anymore
Further coiling was abandoned. Intracranial blood circulation was normal and patient was hemodynamically stable.
DynaCT at end of procedure showing diffuse SAH. Dense contrast is seen in ambient cistern
NCCT head done next morning, patient still intubated, showing diffuse SAH, IVH, e/o residual contrast and significant hydrocephalus
NCCT head, post EVD, which was done immediately after seeing the preceding scan; patient was hemodynamically stable throughout
On day 3, patient was extubated and had bilateral lower limb paresis (2/5) as well as left upper limb paresis (4/5). He was irritable with intermittent comprehension and response. Gradually, over a period of 6-7 days, his neurology improved, however he still had significant left lower limb weakness nad the irritability persisted.
NCCT on day 7 showing near complete resolution of hemorrhage, hydrocephalus still persists
MRI on day 7, done as no focal lesion was seen on the preceding CT, shows hydrocephalus, left temporal region hematoma and underlying parenchymal signal change, but no other focal lesions.
EVD drainage was done for two days, during which time , he improved significantly.
After a total of 2 weeks, he was discharged in a stable condition, with only mild residual weakness in left ankle and slight behavioral change but otherwise with good mental score.
complicated carotid plaque with acute thrombus shows complete resolution of thrombus and plaque stabilisation with medical management
This middle aged patient was admitted with history of sudden onset weakness of the left hand about 8-10 days ago. There was past history of transient numbness of left upper limb lasting for 1-2mins about one month ago. MRI brain revealed multiple acute right fronto-parietal infarcts the arranged as a ‘string of pearls’.
DWI images on day of stroke showing multiple acute infarcts in right frontal and parietal region involving both the cortex as well as the subcortical white matter and centrum semiovale
MRA revealed ~ 70% stenosis of proximal RICA.
CE-MRA MIP image showing signal loss and stenosis at right carotid bulb (hand-marked arrow); remaining neck vessels are normal
Carotid DSA was planned with the aim for revascularization.
Right common carotid artery injection revealed a plaque with filling defect in the RICA just beyond the bifurcation with a meniscus sign (suggestive of fresh intraluminal thrombus), causing a 70% stenosis.
RCCA injection lateral view showing the thrombus and stenosis of the carotid bulb
As there was a fresh intraluminal thrombus, revascularization was deferred in view of a high risk of distal embolization. The patient was kept on medications (heparin for a week, clopidogrel, aspirin, atorvastatin)for a period of 2 weeks.
She had gradual and continuous improvement in power and came for DSA after a month.
DSA this time showed resolution of the thrombus and now only a mild smooth stenosis remained.
Follow up DSA after a month showing mild stenosis with no evidence of thrombus
She has been doing well till now and had near complete recovery of power with no further ischemic neurological events