Interpretation Errors in CT Angiography of the Head and Neck and the Benefit of Double Reading
http://www.ajnr.org/content/32/11/2132.abstract
Interpretation Errors in CT Angiography of the Head and Neck and the Benefit of Double Reading
Abstract
cPAX Aneurysm Treatment System from NeuroVasx
cPAX is a polymeric strand delivered into the aneurysm using a technique similar to currently available platinum coil technologies. cPAX, because of its soft polymeric material, is designed to achieve more complete filling of the aneurysm with the probable benefit of greater long term stability. A significant feature of cPAX in comparison to currently available technologies is that it offers the physician the ability to detach the device at any point versus a fixed detachment zone common in platinum coils. The polymeric material also allows for non-invasive CT and MRI scans with little or no artifact for more accurate patient follow-up assessment.

Monitoring Embolized Brain Aneurysms Without radiation or contrast
researchers from the University of British Columbia have discovered an interesting property of the platinum embolism implant – it can act as a fairly accurate sensor and antenna. The reason is simply that the implant’s coiled shape causes its material properties, namely its resonance frequency, to vary depending on the blood flow through it. A simple handheld RF reader is all that would be required to monitor the status of the embolization-coil sensor.

Department of Electrical & Computer Engineering, University of British Columbia, 2332 Main Mall, Vancouver, BC, V6T 1Z4 Canada. The rupture of a cerebral aneurysm is the most common cause of subarachnoid hemorrhage. Endovascular embolization of the aneurysms by implantation of Guglielmi detachable coils (GDC) has become a major treatment approach in the prevention of a rupture. Implantation of the coils induces formation of tissues over the coils, embolizing the aneurysm. However, blood entry into the coiled aneurysm often occurs due to failures in the embolization process. Current diagnostic methods used for aneurysms, such as X-ray angiography and computer tomography, are ineffective for continuous monitoring of the disease and require extremely expensive equipment. Here we present a novel technique for wireless monitoring of cerebral aneurysms using implanted embolization coils as radiofrequency resonant sensors that detect the blood entry. The experiments show that commonly used embolization coils could be utilized as electrical inductors or antennas. As the blood flows into a coil-implanted aneurysm, parasitic capacitance of the coil is modified because of the difference in permittivity between the blood and the tissues grown around the coil, resulting in a change in the coil's resonant frequency. The resonances of platinum GDC-like coils embedded in aneurysm models are detected to show average responses of 224-819MHz/ml to saline injected into the models. This preliminary demonstration indicates a new possibility in the use of implanted GDC as a wireless sensor for embolization failures, the first step toward realizing long-term, noninvasive, and cost-effective remote monitoring of cerebral aneurysms treated with coil embolization.Radio aneurysm coils for noninvasive detection of cerebral embolization failures: A preliminary study.
Source
Abstract
Nfocus Luna Aneurysm Embolization System
The Luna AES treats brain aneurysms by blocking (embolizing) blood flow while providing a scaffold to encourage tissue growth across an aneurysm opening and create a plug. The Luna uses a self-expandable, multi-layer oval implant made from Nitinol, a nickel-titanium alloy. The properties of the device allow it to easily compress within a conventional catheter, and then rapidly and easily open to full size once deployed within an aneurysm.

The Safety of Intravenous Thrombolysis for Ischemic Stroke in Patients With ...
Sent to you by subbu via Google Reader:
Background and Purpose—
Unruptured cerebral aneurysms are currently considered a contraindication to intravenous tissue-type plasminogen activator for acute ischemic stroke. This is due to a theoretical increase in the risk of hemorrhage from aneurysm rupture, although it is unknown whether this risk is a significant one. We sought to determine the safety of intravenous tissue-type plasminogen activator administration in a cohort of patients with pre-existing aneurysms.
Methods—We reviewed the medical records of patients treated for acute ischemic stroke with intravenous tissue-type plasminogen activator during an 11-year period at 2 academic medical centers. We identified a subset of patients with unruptured cerebral aneurysms present on prethrombolysis vascular imaging. Our outcomes of interest were any intracranial hemorrhage, symptomatic intracranial hemorrhage, and subarachnoid hemorrhage. Fisher exact test was used to compare the rates of hemorrhage among patients with and without aneurysms.
Results—We identified 236 eligible patients, of whom 22 had unruptured cerebral aneurysms. The rate of intracranial hemorrhage among patients with aneurysms (14%; 95% CI, 3%–35%) did not significantly differ from the rate among patients without aneurysms (19%; 95% CI, 14%–25%). None of the patients with aneurysms developed symptomatic intracranial hemorrhage (0%; 95% CI, 0%–15%) compared with 10 of 214 patients without aneurysms (5%; 95% CI, 2%–8%). Similar proportions of patients developed subarachnoid hemorrhage (5%; 95% CI, 0%–23% versus 6%; 95% CI, 3%–10%).
Conclusions—Our findings suggest that intravenous tissue-type plasminogen activator for acute ischemic stroke is safe to administer in patients with pre-existing cerebral aneurysms because the risk of aneurysm rupture and symptomatic intracranial hemorrhage is low.
Things you can do from here:
- Subscribe to Stroke ASAP using Google Reader
- Get started using Google Reader to easily keep up with all your favorite sites
Dural venous sinus angioplasty and stenting for the treatment of idiopathic intracranial hypertension
Background
Lumboperitoneal shunt (LPS), ventriculoperitoneal shunt (VPS) and optic nerve sheath fenestration (ONSF) are accepted surgical therapies for medically refractory idiopathic intracranial hypertension (IIH). In the subset of patients with IIH and venous sinus stenosis, dural venous sinus stenting has emerged as an alternative surgical approach.
MethodsAll cases of dural stents for IIH at our institution were retrospectively reviewed. Eligibility criteria included medically refractory IIH with documented papilledema and dural venous sinus stenosis of the dominant venous outflow system (gradient ≥10 mm Hg).
ResultsFifteen cases (all women) of mean age 34 years were identified. All had failed medical therapy and six had failed surgical intervention. Technical success was achieved in all patients without major periprocedural complications. The mean preprocedural gradient across the venous stenosis was reduced from 24 mm Hg before the procedure to 4 mm Hg after the procedure. Headache resolved or improved in 10 patients. Papilledema resolved in all patients and visual acuity stabilized or improved in 14 patients. There were no instances of restenosis among the 14 patients with follow-up imaging.
ConclusionIn this small case series, dural sinus stenting for IIH was performed safely with a high degree of technical success and with excellent clinical outcomes. These results suggest that angioplasty and stenting for the treatment of medically refractory IIH in patients with dural sinus stenosis warrants further investigation as an alternative to LPS, VPS and ONSF.
Mechanical thrombectomy as first-line treatment for venous sinus thrombosis: technical considerations and preliminary results using the AngioJet devic
Mechanical thrombectomy as first-line treatment for venous sinus thrombosis: technical considerations and preliminary results using the AngioJet device
Cerebral venous sinus thrombosis (CVT) is an uncommon cause of stroke that is usually treated medically with intravenous heparin therapy followed by long-term anticoagulation therapy. A series of patients with CVT who underwent rheolytic thrombectomy with the AngioJet as a first-line adjunctive treatment in addition to standard anticoagulation therapy is presented.
MethodsProspectively maintained endovascular databases at two institutions were retrospectively reviewed. The available clinical and imaging data were compiled at each institution and combined for analysis.
ResultsOver 18 months, 13 patients (seven women and six men; age range 17–73 years, median age 45 years) with CVT were treated with rheolytic thrombectomy. Immediate (partial or complete) recanalization of the thrombosed intracranial sinuses was achieved in all patients. At a median radiographic follow-up of 7 months there was continued patency of all recanalized sinuses. Clinical follow-up was available on nine patients: modified Rankin score of 0 in four patients, 1 in three patients and 6 in two patients.
ConclusionThis series demonstrates the feasibility of performing mechanical thrombectomy as a first-line treatment for acute CVT. This technique facilitates the prompt restoration of intracranial venous outflow, which may result in rapid neurological and symptomatic improvement.
Interventional Stroke Therapies in the Elderly: Are We Helping?
Interventional Stroke Therapies in the Elderly: Are We Helping?
- Louise D. McCullough, MD, PhD, The Stroke Clinic at Hartford Hospital, 80 Seymour St, Suite JB603, Hartford, CT 06102; e-mail:lmccullough@uchc.edu
Abstract
BACKGROUND AND PURPOSE: It is unclear whether endovascular therapies for the treatment of AIS are being offered or are safe in older adults. The use and safety of endovascular interventions in patients older than 75 years of age were assessed.
MATERIALS AND METHODS: A retrospective review of patients with AIS 75 years or older (n = 37/1064) was compared with a younger cohort (n = 70/1190) by using an established data base. Admission and discharge NIHSS scores, rates of endovascular treatment, SICH, in-hospital mortality, and the mBI were assessed.
RESULTS: Rates of endovascular treatments were significantly lower in older patients (5.9% in the younger-than-75-year versus 3.5% in the older-than-75-year cohort, P = .007). Stroke severity as measured by the NIHSS score was equivalent in the 2 age groups. The mBI at 12 months was worse in the older patients (mild or no disability in 52% of the younger-than-75-year and 22% in the 75-year-or-older cohort, P = .006). Older patients had higher rates of SICH (9% in younger-than-75-year versus 24% in the 75-year-or-older group, P = .04) and in-hospital mortality (26% in younger-than-75-year versus 46% in the 75-year-or-older group, P = .05).
CONCLUSIONS: Patients older than 75 years of age were less likely to receive endovascular treatments. Older patients had higher rates of SICH, disability, and mortality. Prospective randomized trials are needed to determine the criteria for selecting patients most likely to benefit from acute endovascular therapies.
Abbreviations
- AIS
- acute ischemic stroke
- HIAT
- Houston intra-arterial therapy
- IA
- intra-arterial
- ICH
- intracranial hemorrhage
- INR
- international normalized ratio
- IQR
- interquartile range
- LDL
- low-density lipoprotein
- mBI
- modified Barthel Index
- SICH
- symptomatic intracranial hemorrhage
- TIMI
- thrombolysis in myocardial infarction
Extending the Time Window for Endovascular Procedures According to Collateral Pial Circulation [Original Contributions; Clinical Sciences]
Extending the Time Window for Endovascular Procedures According to Collateral Pial Circulation [Original Contributions; Clinical Sciences]: Background and Purpose—
Good collateral pial circulation (CPC) predicts a favorable outcome in patients undergoing intra-arterial procedures. We aimed to determine if CPC status may be used to decide about pursuing recanalization efforts.
Methods—
Pial collateral score (0–5) was determined on initial angiogram. We considered good CPC when pial collateral score <3, defined total time of ischemia (TTI) as onset-to-recanalization time, and clinical improvement >4-point decline in admission–discharge National Institutes of Health Stroke Scale.
Results—
We studied CPC in 61 patients (31 middle cerebral artery, 30 internal carotid artery). Good CPC patients (n=21 [34%]) had lower discharge National Institutes of Health Stroke Scale score (7 versus 21; P=0.02) and smaller infarcts (56 mL versus 238 mL; P<0.001). In poor CPC patients, a receiver operating characteristic curve defined a TTI cutoff point <300 minutes (sensitivity 67%, specificity 75%) that better predicted clinical improvement (TTI <300: 66.7% versus TTI >300: 25%; P=0.05). For good CPC patients, no temporal cutoff point could be defined. Although clinical improvement was similar for patients recanalizing within 300 minutes (poor CPC: 60% versus good CPC: 85.7%; P=0.35), the likelihood of clinical improvement was 3-fold higher after 300 minutes only in good CPC patients (23.1% versus 90.1%; P=0.01). Similarly, infarct volume was reduced 7-fold in good as compared with poor CPC patients only when TTI >300 minutes (TTI <300: poor CPC: 145 mL versus good CPC: 93 mL; P=0.56 and TTI >300: poor CPC: 217 mL versus good CPC: 33 mL; P<0.01). After adjusting for age and baseline National Institutes of Health Stroke Scale score, TTI <300 emerged as an independent predictor of clinical improvement in poor CPC patients (OR, 6.6; 95% CI, 1.01–44.3; P=0.05) but not in good CPC patients. In a logistic regression, good CPC independently predicted clinical improvement after adjusting for TTI, admission National Institutes of Health Stroke Scale score, and age (OR, 12.5; 95% CI, 1.6–74.8; P=0.016).
Conclusions—
Good CPC predicts better clinical response to intra-arterial treatment beyond 5 hours from onset. In patients with stroke receiving endovascular treatment, identification of good CPC may help physicians when considering pursuing recanalization efforts in late time windows.
Risk Profile of Intracranial Aneurysms: Rupture Rate Is Not Constant After Formation [Original Contributions; Clinical Sciences]
Wonderful article
this was always suspected or rather known that small aneurysms do rupture but the prospective trials could not show this. Sato et al have now come with this article and proven statistically that some aneurysms form and rupture soon after while others remain stable and do not rupture for long.
Management of asymptomatic unruptured intracranial aneurysms remains controversial, and recent prospective follow-up studies showed that the rupture rate of small aneurysms is very low. These results are inconsistent with the finding that the majority of ruptured aneurysms in patients with subarachnoid hemorrhage are small.
Methods—
A Markov model was constructed to simulate the natural history of intracranial aneurysms. All epidemiological and statistical data obtained from the Portal Site of Official Statistics of Japan (e-Stat) were adjusted to the standardized age distribution. From the selected data of aneurysm formation, the prevalence of unruptured aneurysms was estimated as 1.45% and the incidence of subarachnoid hemorrhage calculated to be 19.7/100 000/year in the whole standardized population.
Results—
The function for rupture rate constant with time was first analyzed. Selected values for annual rupture rates of 0.3%, 0.5%, 0.7%, and 1.0% showed inconsistencies in the relationship between the prevalence of unruptured aneurysm and the incidence of subarachnoid hemorrhage. Next, the function for a short period of high risk followed by a long period of low risk was considered. Annual rupture rates of 0.5%, 0.7%, and 1.0% indicated epidemiological compatibility with additional early rupture rates of 20%, 15%, and 10%, respectively.
Conclusions—
This study suggests that some aneurysms bleed shortly after formation and thus are rarely detected as unruptured aneurysms. Most aneurysms without early rupture remain stable for the remainder of life through some healing process, and prophylactic treatment for incidentally identified small unruptured aneurysms has no rationale.
Neurogenic pulmonary edema after rupture of intracranial aneurysm during endovascular coiling
Click to read full article on pubmed central website
Accuracy of On-Call Resident Interpretation of CT Angiography for Intracrani...
While radiology residents are pretty good in reporting in general, they lack the skills in vascular imaging and neuroradiology in general.
OBJECTIVE. The purpose of this article is to evaluate the accuracy of preliminary on-call radiology resident interpretation of CT angiography (CTA) compared with digital subtraction angiography (DSA) in detecting cerebral aneurysms in subarachnoid hemorrhage (SAH).
MATERIALS AND METHODS. A retrospective review compared resident interpretations of head CTA performed after hours for SAH to the results of DSA. The sensitivity and specificity of resident interpretations were classified on a per-patient and per-aneurysm basis. The accuracy of resident interpretations was also determined according to aneurysm location and number.
RESULTS. Between January 2007 and December 2009, 83 patients with SAH underwent both CTA and DSA. DSA documented an aneurysm in 53 of 83 patients. Per patient, residents identified at least one aneurysm in 46 of 53 patients (87%). Per aneurysm, resident sensitivity and specificity for detecting aneurysms of any size were 62% and 91%, respectively, which improved for aneurysms 3 mm or larger to 73% and 97%, respectively. The posterior communicating and intracranial internal carotid arteries were resident "blind spots," with aneurysms 3 mm or larger detected with sensitivities of 33% and 50%, respectively. In contrast, anterior communicating artery aneurysms were correctly identified 95% of the time. In only 35% of cases with multiple aneurysms did residents correctly identify more than one aneurysm.
CONCLUSION. The sensitivity of on-call resident interpretation of CTA for aneurysms in SAH is lower than expected, with a potential for delay in diagnosis and management in a small number of patients. Focused training to carefully review apparent blind spots and the frequency of multiple aneurysms may reduce inaccuracies.
Interventional Stroke Therapies in the Elderly: Are We Helping?
BACKGROUND AND PURPOSE:
It is unclear whether endovascular therapies for the treatment of AIS are being offered or are safe in older adults. The use and safety of endovascular interventions in patients older than 75 years of age were assessed.
MATERIALS AND METHODS:
A retrospective review of patients with AIS 75 years or older (n = 37/1064) was compared with a younger cohort (n = 70/1190) by using an established data base. Admission and discharge NIHSS scores, rates of endovascular treatment, SICH, in-hospital mortality, and the mBI were assessed.
RESULTS:
Rates of endovascular treatments were significantly lower in older patients (5.9% in the younger-than-75-year versus 3.5% in the older-than-75-year cohort, P = .007). Stroke severity as measured by the NIHSS score was equivalent in the 2 age groups. The mBI at 12 months was worse in the older patients (mild or no disability in 52% of the younger-than-75-year and 22% in the 75-year-or-older cohort, P = .006). Older patients had higher rates of SICH (9% in younger-than-75-year versus 24% in the 75-year-or-older group, P = .04) and in-hospital mortality (26% in younger-than-75-year versus 46% in the 75-year-or-older group, P = .05).
CONCLUSIONS:
Patients older than 75 years of age were less likely to receive endovascular treatments. Older patients had higher rates of SICH, disability, and mortality. Prospective randomized trials are needed to determine the criteria for selecting patients most likely to benefit from acute endovascular therapies.
Pediatric Intracranial Aneurysms: New and Enlarging Aneurysms after Index Aneurysm Treatment or Observation [PEDIATRICS]
Children with brain aneurysms may be at higher risk than adults to develop new or enlarging aneurysms in a relatively short time. We sought to identify comorbidities and angiographic features in children that predict new aneurysm formation or enlargement of untreated aneurysms.
MATERIALS AND METHODS:Retrospective analysis of the University of California–San Francisco Pediatric Aneurysm Cohort data base including medical records and imaging studies was performed.
RESULTS:Of 83 patients harboring 114 intracranial aneurysms not associated with brain arteriovenous malformations or intracranial arteriovenous fistulas, 9 (8.4%) developed new or enlarging brain aneurysms an average of 4.2 years after initial presentation. Comorbidities that may be related to aneurysm formation were significantly higher in patients who developed new aneurysms (89%) as opposed to patients who did not develop new or enlarging aneurysms (41%; RR, 9.5; 95% CI, 1.9%–48%; P = .0099). Patients with multiple aneurysms at initial presentation were more likely than patients with a single aneurysm at presentation to develop a new or enlarging aneurysm (RR, 6.2; 95% CI, 2.1%–185; P = .0058). Patients who initially presented with at least 1 fusiform aneurysm were more likely to develop a new or enlarging aneurysm than patients who did not present with a fusiform aneurysm (RR, 22; 95% CI, 3.6%–68%; P = .00050). Index aneurysm treatment with parent artery occlusion also was associated with higher risk of new aneurysm formation (RR, 4.2; 95% CI, 1.3%–13%; P = .024). New aneurysms did not necessarily arise near index aneurysms. The only fatality in the series was due to subarachnoid hemorrhage from a new posterior circulation aneurysm arising 20 months after index anterior circulation aneurysm treatment in an immunosuppressed patient.
CONCLUSIONS:Patients who presented with a fusiform aneurysm had a significantly greater incidence of developing a new aneurysm or enlargement of an index aneurysm than did those who presented with a saccular aneurysm. In our patient cohort, 8 of the 9 children who eventually developed new or enlarging brain aneurysms initially presented with fusiform aneurysm morphology. Other comorbidities or multiple aneurysms were also common in these patients at initial presentation.
Cerebral Perfusion Long Term after Therapeutic Occlusion of the Internal Carotid Artery in Patients Who Tolerated Angiographic Balloon Test Occlusion
Cerebral Perfusion Long Term after Therapeutic Occlusion of the Internal Carotid Artery in Patients Who Tolerated Angiographic Balloon Test Occlusion
Gevers, S., Heijtel, D., Ferns, S. P., van Ooij, P., van Rooij, W. J., van Osch, M. J., van den Berg, R., Nederveen, A. J., Majoie, C. B.
Therapeutic carotid occlusion is an established technique for treatment of large and giant aneurysms of the ICA, in patients with synchronous venous filling on angiography during BTO. Concern remains that hemodynamic alterations after permanent occlusion will predispose the patient to new ischemic injury in the ipsilateral hemisphere. The purpose of this study was to assess whether BTO with synchronous venous filling is associated with normal CBF long term after carotid sacrifice.
MATERIALS AND METHODS:Eleven patients were included (all women; mean age, 50.5 years; mean follow-up, 38.5 months). ASL with single and multiple TIs was used to assess CBF and its temporal characteristics. Selective ASL was used to assess actual territorial contribution of the ICA and BA. Collateral flow via the AcomA or PcomA or both was determined by time-resolved 3D PCMR. Paired t tests were used to compare CBF and timing parameters between hemispheres.
RESULTS:Absolute CBF values were within the normal range. There was no significant CBF difference between hemispheres ipsilateral and contralateral to carotid sacrifice (49.4 ± 11.2 versus 50.1 ± 10.1 mL/100 g/min). Arterial arrival time and trailing edge time were significantly prolonged on the occlusion side (816 ± 119 ms versus 741 ± 103 ms, P = .001; and 1765 ± 179 ms versus 1646 ± 190 ms, P < .001). Two patients had collateral flow through the AcomA only and were found to have increased timing parameters compared with 9 patients with mixed collateral flow through both the AcomA and PcomA.
CONCLUSIONS:In this small study, patients with synchronous venous filling during BTO had normal CBF long term after therapeutic ICA occlusion.
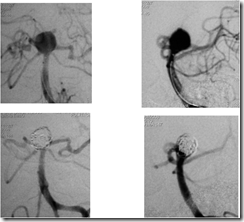
Stent assisted coiling of wide neck basilar tip aneurysm
This is the case of a middle aged patient with Fisher grade 3, Hunt and Hess grade 2 subarachnoid haemorrhage with a ruptured basilar tip aneurysm. The aneurysm was moderate sized, with a wide neck ~ 7 mm involving both the proximal p1 PCA segments (left more than right), and directed posterosuperiorly. The Pcoms were seen although not very prominent.
An Enterprise 5.5 x 22 mm stent was passed via a Prowler Select Plus microcatheter across the aneurysm neck into the left PCA with trailing portion kept in the basilar artery. A SL 10 microcatheter was then navigated and placed in the aneurysm fundus. The stent was partially opened (JAILING technique) and coiling done. Good packing of the aneurysm was achieved. Then the stent was fully deployed and left in situ.
The patient had been prepared with 300 mg Aspirin and 300 mg Clopidogrel prior to the procedure and given 5000 U heparin bolus after sheath placement. A single femoral puncture had been done with 6F sheath placement and a 6F Envoy used as guide catheter. A double Y Tuohy Borst hemostatic adapter was used to pass the stent and coil noth through the same guide catheter.
The patient had an uneventful recovery and was discharged in stable condition.
She was advised to have Aspirin 150 mg and Clopidogrel 75 mg once daily for next three months and then Aspirin 150 mg for life.
Fig 1. Frontal and Lateral views of LVA injection
Fig 2. 3D DSA images of LVA injection
Fig 3. Stent placement in the left PCA across the aneurysm neck
Fig 4. Coiling of the aneurysm
Fig 5. The deployed stent and fully coiled aneurysm
Fig 6. Pre and post procedure comparative angiograms