Accuracy of On-Call Resident Interpretation of CT Angiography for Intracrani...
While radiology residents are pretty good in reporting in general, they lack the skills in vascular imaging and neuroradiology in general.
OBJECTIVE. The purpose of this article is to evaluate the accuracy of preliminary on-call radiology resident interpretation of CT angiography (CTA) compared with digital subtraction angiography (DSA) in detecting cerebral aneurysms in subarachnoid hemorrhage (SAH).
MATERIALS AND METHODS. A retrospective review compared resident interpretations of head CTA performed after hours for SAH to the results of DSA. The sensitivity and specificity of resident interpretations were classified on a per-patient and per-aneurysm basis. The accuracy of resident interpretations was also determined according to aneurysm location and number.
RESULTS. Between January 2007 and December 2009, 83 patients with SAH underwent both CTA and DSA. DSA documented an aneurysm in 53 of 83 patients. Per patient, residents identified at least one aneurysm in 46 of 53 patients (87%). Per aneurysm, resident sensitivity and specificity for detecting aneurysms of any size were 62% and 91%, respectively, which improved for aneurysms 3 mm or larger to 73% and 97%, respectively. The posterior communicating and intracranial internal carotid arteries were resident "blind spots," with aneurysms 3 mm or larger detected with sensitivities of 33% and 50%, respectively. In contrast, anterior communicating artery aneurysms were correctly identified 95% of the time. In only 35% of cases with multiple aneurysms did residents correctly identify more than one aneurysm.
CONCLUSION. The sensitivity of on-call resident interpretation of CTA for aneurysms in SAH is lower than expected, with a potential for delay in diagnosis and management in a small number of patients. Focused training to carefully review apparent blind spots and the frequency of multiple aneurysms may reduce inaccuracies.
Interventional Stroke Therapies in the Elderly: Are We Helping?
BACKGROUND AND PURPOSE:
It is unclear whether endovascular therapies for the treatment of AIS are being offered or are safe in older adults. The use and safety of endovascular interventions in patients older than 75 years of age were assessed.
MATERIALS AND METHODS:
A retrospective review of patients with AIS 75 years or older (n = 37/1064) was compared with a younger cohort (n = 70/1190) by using an established data base. Admission and discharge NIHSS scores, rates of endovascular treatment, SICH, in-hospital mortality, and the mBI were assessed.
RESULTS:
Rates of endovascular treatments were significantly lower in older patients (5.9% in the younger-than-75-year versus 3.5% in the older-than-75-year cohort, P = .007). Stroke severity as measured by the NIHSS score was equivalent in the 2 age groups. The mBI at 12 months was worse in the older patients (mild or no disability in 52% of the younger-than-75-year and 22% in the 75-year-or-older cohort, P = .006). Older patients had higher rates of SICH (9% in younger-than-75-year versus 24% in the 75-year-or-older group, P = .04) and in-hospital mortality (26% in younger-than-75-year versus 46% in the 75-year-or-older group, P = .05).
CONCLUSIONS:
Patients older than 75 years of age were less likely to receive endovascular treatments. Older patients had higher rates of SICH, disability, and mortality. Prospective randomized trials are needed to determine the criteria for selecting patients most likely to benefit from acute endovascular therapies.
Pediatric Intracranial Aneurysms: New and Enlarging Aneurysms after Index Aneurysm Treatment or Observation [PEDIATRICS]
Children with brain aneurysms may be at higher risk than adults to develop new or enlarging aneurysms in a relatively short time. We sought to identify comorbidities and angiographic features in children that predict new aneurysm formation or enlargement of untreated aneurysms.
MATERIALS AND METHODS:Retrospective analysis of the University of California–San Francisco Pediatric Aneurysm Cohort data base including medical records and imaging studies was performed.
RESULTS:Of 83 patients harboring 114 intracranial aneurysms not associated with brain arteriovenous malformations or intracranial arteriovenous fistulas, 9 (8.4%) developed new or enlarging brain aneurysms an average of 4.2 years after initial presentation. Comorbidities that may be related to aneurysm formation were significantly higher in patients who developed new aneurysms (89%) as opposed to patients who did not develop new or enlarging aneurysms (41%; RR, 9.5; 95% CI, 1.9%–48%; P = .0099). Patients with multiple aneurysms at initial presentation were more likely than patients with a single aneurysm at presentation to develop a new or enlarging aneurysm (RR, 6.2; 95% CI, 2.1%–185; P = .0058). Patients who initially presented with at least 1 fusiform aneurysm were more likely to develop a new or enlarging aneurysm than patients who did not present with a fusiform aneurysm (RR, 22; 95% CI, 3.6%–68%; P = .00050). Index aneurysm treatment with parent artery occlusion also was associated with higher risk of new aneurysm formation (RR, 4.2; 95% CI, 1.3%–13%; P = .024). New aneurysms did not necessarily arise near index aneurysms. The only fatality in the series was due to subarachnoid hemorrhage from a new posterior circulation aneurysm arising 20 months after index anterior circulation aneurysm treatment in an immunosuppressed patient.
CONCLUSIONS:Patients who presented with a fusiform aneurysm had a significantly greater incidence of developing a new aneurysm or enlargement of an index aneurysm than did those who presented with a saccular aneurysm. In our patient cohort, 8 of the 9 children who eventually developed new or enlarging brain aneurysms initially presented with fusiform aneurysm morphology. Other comorbidities or multiple aneurysms were also common in these patients at initial presentation.
Cerebral Perfusion Long Term after Therapeutic Occlusion of the Internal Carotid Artery in Patients Who Tolerated Angiographic Balloon Test Occlusion
Cerebral Perfusion Long Term after Therapeutic Occlusion of the Internal Carotid Artery in Patients Who Tolerated Angiographic Balloon Test Occlusion
Gevers, S., Heijtel, D., Ferns, S. P., van Ooij, P., van Rooij, W. J., van Osch, M. J., van den Berg, R., Nederveen, A. J., Majoie, C. B.
Therapeutic carotid occlusion is an established technique for treatment of large and giant aneurysms of the ICA, in patients with synchronous venous filling on angiography during BTO. Concern remains that hemodynamic alterations after permanent occlusion will predispose the patient to new ischemic injury in the ipsilateral hemisphere. The purpose of this study was to assess whether BTO with synchronous venous filling is associated with normal CBF long term after carotid sacrifice.
MATERIALS AND METHODS:Eleven patients were included (all women; mean age, 50.5 years; mean follow-up, 38.5 months). ASL with single and multiple TIs was used to assess CBF and its temporal characteristics. Selective ASL was used to assess actual territorial contribution of the ICA and BA. Collateral flow via the AcomA or PcomA or both was determined by time-resolved 3D PCMR. Paired t tests were used to compare CBF and timing parameters between hemispheres.
RESULTS:Absolute CBF values were within the normal range. There was no significant CBF difference between hemispheres ipsilateral and contralateral to carotid sacrifice (49.4 ± 11.2 versus 50.1 ± 10.1 mL/100 g/min). Arterial arrival time and trailing edge time were significantly prolonged on the occlusion side (816 ± 119 ms versus 741 ± 103 ms, P = .001; and 1765 ± 179 ms versus 1646 ± 190 ms, P < .001). Two patients had collateral flow through the AcomA only and were found to have increased timing parameters compared with 9 patients with mixed collateral flow through both the AcomA and PcomA.
CONCLUSIONS:In this small study, patients with synchronous venous filling during BTO had normal CBF long term after therapeutic ICA occlusion.
Stent assisted coiling of wide neck basilar tip aneurysm
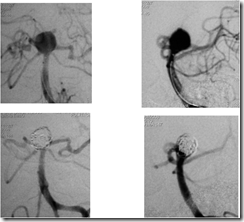
This is the case of a middle aged patient with Fisher grade 3, Hunt and Hess grade 2 subarachnoid haemorrhage with a ruptured basilar tip aneurysm. The aneurysm was moderate sized, with a wide neck ~ 7 mm involving both the proximal p1 PCA segments (left more than right), and directed posterosuperiorly. The Pcoms were seen although not very prominent.
An Enterprise 5.5 x 22 mm stent was passed via a Prowler Select Plus microcatheter across the aneurysm neck into the left PCA with trailing portion kept in the basilar artery. A SL 10 microcatheter was then navigated and placed in the aneurysm fundus. The stent was partially opened (JAILING technique) and coiling done. Good packing of the aneurysm was achieved. Then the stent was fully deployed and left in situ.
The patient had been prepared with 300 mg Aspirin and 300 mg Clopidogrel prior to the procedure and given 5000 U heparin bolus after sheath placement. A single femoral puncture had been done with 6F sheath placement and a 6F Envoy used as guide catheter. A double Y Tuohy Borst hemostatic adapter was used to pass the stent and coil noth through the same guide catheter.
The patient had an uneventful recovery and was discharged in stable condition.
She was advised to have Aspirin 150 mg and Clopidogrel 75 mg once daily for next three months and then Aspirin 150 mg for life.
Fig 1. Frontal and Lateral views of LVA injection
Fig 2. 3D DSA images of LVA injection
Fig 3. Stent placement in the left PCA across the aneurysm neck
Fig 4. Coiling of the aneurysm
Fig 5. The deployed stent and fully coiled aneurysm
Fig 6. Pre and post procedure comparative angiograms
Regional Leptomeningeal Score on CT Angiography Predicts Clinical and Imaging Outcomes in Patients with Acute Anterior Circulation Occlusions
In this article from Alberta, an objective scoring system with clincal correlation has been published and is welcome. It should pave the path for better non-invasive assessment of the patient.